Scleral Fixation of a Single-Piece AcrySof Toric Intraocular Lens: A Case Report
Article information
Abstract
Purpose
To describe a simple and least invasive surgical method of transscleral fixation of a dislocated single-piece AcrySof® toric intraocular lens (IOL).
Case summary
A 62-year-old male was referred with dislocated toric IOL (SN6AT4, AcrySof® IQ Toric; Alcon Laboratories, Fort Worth, TX, USA) in his right eye after an uneventful cataract surgery. Scleral fixation using the toric IOL was performed by placing the suture knot at the optic-haptic junction right beside the toric axis markings which easily achieved the desired positioning of the axis. The preoperative uncorrected distance visual acuity was 20/400 and it improved to 20/60 at 1 week after repositioning of the IOL and the IOL was well-centered with its toric alignment within 5 degrees of the intended axis.
Conclusions
Transscleral fixation of single-piece AcrySof toric IOLs is easy to learn technique, which reduces surgical time with minimal manipulation and enables IOL stability with good postoperative toric axis alignment.
INTRODUCTION
Recently cataract surgery has evolved to a refractive surgery due to the technical advances in premium intraocular lenses (IOLs) such as multifocal and toric IOLs. Implantation of a toric IOL enabled patients with astigmatism to achieve optimal distance vision without the use of spectacles after cataract surgery. The introduction of multifocal toric IOLs made patients spectacle-free not only in distance vision, but also for near and intermediate vision.
IOL dislocation is an uncommon late complication of cataract surgery. The cumulative incidence over 10 years was 1% in one study [1]. The cumulative risk of IOL dislocation did not significantly increase with time showing 0.1, 0.1, 0.2, 0.7, and 1.7% incidence in 5, 10, 15, 20, and 25 years, respectively [2]. The major predisposing factors of late IOL dislocation were pseudoexfoliation, glaucoma and zonular dehiscence at the time of cataract surgery [3].
A dislocated IOL often requires surgical intervention; explantation and exchange of the IOL or repositioning of the IOL. Although surgical outcomes and complications showed no difference between the two surgical interventions [4,5], IOL repositioning should be considered first unless IOL exchange is necessary due to complications of the IOL itself as IOL explantation is a more complicated procedure. Especially in a situation of a dislocated premium IOL, the patients’ demand on repositioning seems to be above explantation and exchange of the pre-existing IOL. This may be affected by the high cost of the premium IOLs and the visual demands of patients who had these IOLs implanted.
This case presents a simple, minimally invasive and easy to learn technique of IOL scleral fixation which can also achieve desired axis alignment with good rotational stability. This report was approved by the Institutional Review Board of Soonchunhyang University Seoul Hospital (No. 2023-12-004), with a waiver for informed consent.
CASE
A 62-year-old male was referred with a dislocated toric IOL (SN6AT4, AcrySof® IQ Toric; Alcon Laboratories, Inc., Fort Worth, TX, USA) in his right eye. He had zonular dialysis with vitreous prolapse in the anterior chamber since 3 months prior to the referral after an uneventful cataract surgery performed 14 months ago. A simple and minimally invasive surgical method to reposition the dislocated IOL was used in this patient.
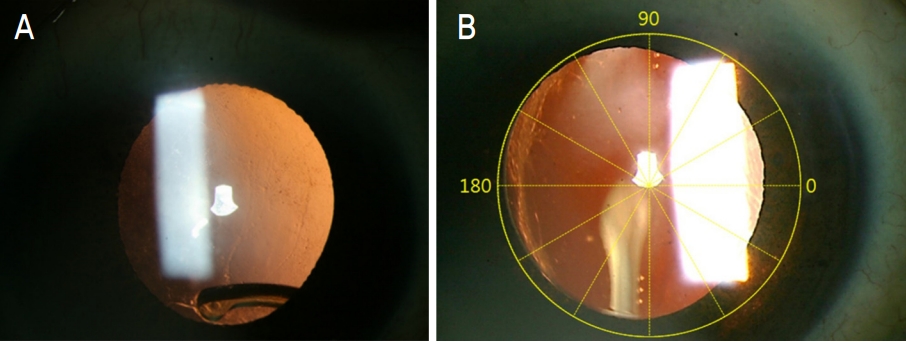
The surgical technique was targeted to achieve desired toric axis alignment with stability to reposition a dislocated or decentered toric IOL. The IOL has a notch on its optic-haptic junction which is just beside the toric markings on the optic (Fig. 1). Since this notch is aligned in its toric axis, this part was used as the suture fixation point on the IOL and fixated the other end of the suture at the sclera on the same axis as the corneal marking for toric IOL placement (Fig. 2).

A schematic drawing of a single-piece AcrySof toric intraocular lens. There is a notch at the optic-haptic junction right beside the toric markings.
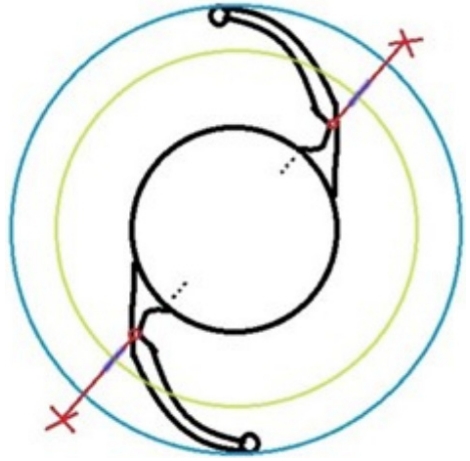
The position of the scleral fixation suture (X), when sutured along the corneal axis markings, the toric axis of the intraocular lens nearly meets the target alignment with its other end fixated at the notch of the haptic (green circle: imaginary limbus, blue circle: imaginary sulcus).
After a drop of topical 4% lidocaine was administered to numb the surface of the eye, the toric axis was marked on the cornea limbus. Then two fornix-based conjunctival peritomies were made on the toric axis 180° apart (Fig. 3A). Pinpoint anesthesia was done by injecting 2 mL of 4% Lidocaine through this opening by passing a blunt 27-gauge cannula along the globe towards the posterior sub-Tenon’s space of the eye. Three corneal stab incisions were made with beaver blade; first on the inferotemporal side for the infusion cannula to maintain the anterior chamber during manipulation of the IOL, second on 3 o’clock site and third on 12 o’clock site to rotate and manipulate the IOL (Fig. 3B). The IOL was rotated and placed above the iris plane using a Sinskey hook and a lens hook (Fig. 3C). The 12 o’clock corneal incision site was slightly enlarged with the beaver blade and anterior vitrectomy was performed using a 25-gauge vitreous cutter through this opening to remove the remnant lens capsule and prolapsed vitreous interrupting IOL centration (Fig. 3D). One arm of a double-armed 10-0 prolene (PROLENE® Polypropylene Suture; Ethicon, Somerville, NJ, USA) suture with a long-curved needle was passed approximately 2-3 mm posterior to the limbus marking and docked into a 26-gauge hollow needle passed in a similar fashion from the opposite side (Fig. 3E). The 26-gauge needle with the 10-0 prolene suture was then withdrawn resulting in the 10-0 prolene suture bridging the posterior form a c-shaped hook) and cut (Fig. 3F). Then the IOL was rotated to place one end of the haptic at the corneal incision site and the haptic was externalized using McPherson tooth forceps (Fig. 3G). The soft and flexible nature of the haptic made it easy to pull out through a small incision without any damage to the haptic. One end of the 10-0 prolene suture was tied at the optic-haptic junction of the temporary externalized haptic. The notch made the suture to be placed more securely, preventing slippage of the knot. The IOL was rotated and the other haptic was externalized by the same method to place the 10-0 prolene knot (Fig. 3H). After placing the IOL in the posterior chamber with its haptics in the ciliary sulcus, tension was adjusted as necessary to center the IOL and the needle of each arm of the suture was passed partially through the sclera to form a loop (Fig. 3I). The needle was then cut off and the suture end was tied firmly to the loop (Fig. 3J). The toric alignment of the IOL matched with the corneal marking for toric IOL placement. The infusion cannula was removed and the corneal incision sites were closed by stromal hydration. Conjunctival peritomy sites were tightly approximated with 8-0 vicryl suture (Fig, 3K) with suture knots of 10-0 prolene securely placed underneath the conjunctiva and Tenon’s fascia (Fig. 3L).
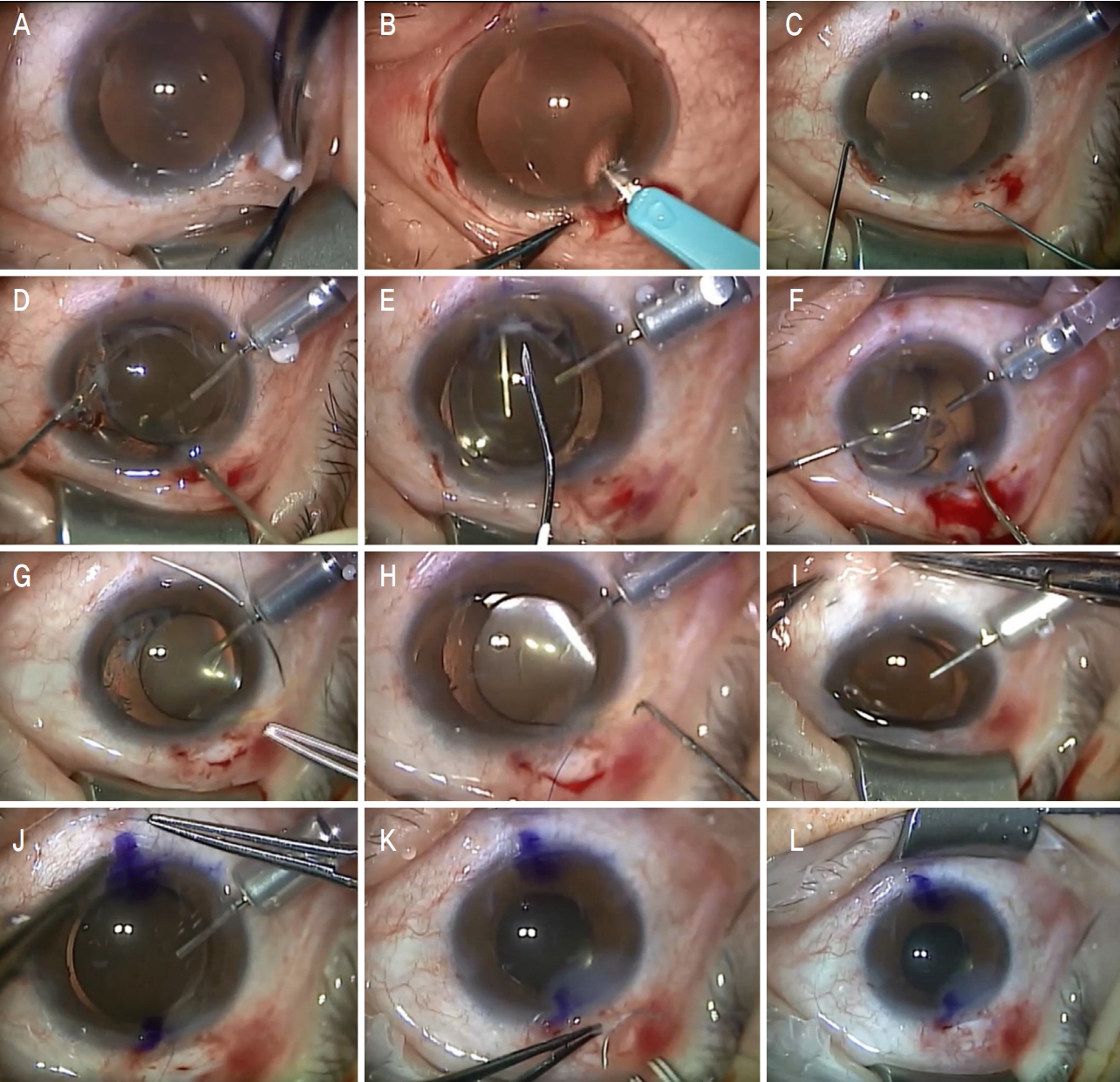
Intraoperative photos to describe the surgical procedure. After two fornix-based conjunctival peritomies were made on the toric axis 180° apart (A), three corneal stab incisions were made with beaver blade; one for infusion cannula, other two for instruments to manipulate the intraocular lens (IOL) (B). The IOL was lifted and placed on the iris plane to prevent IOL drop into the vitreous cavity using a Sinskey hook and a lens hook (C). Then prolapsed vitreous and remnant lens capsule was removed by 25-gauge vitreous cutter (D). One arm of a double-armed 10-0 prolene suture on a long-curved needle was passed approximately 2-3 mm posterior to the limbus and a 26-gauge hollow needle passed in a similar fashion from the opposite side was used for delivering the needle to the opposite side (E). The 10-0 prolene suture bridging the posterior chamber was externalized through the 12 o’clock corneal incision site using a bent 26-gauge needle (F). Each haptic was externalized and each cut end of 10-0 prolene was tied firmly around the notch on the haptic (G, H). After placing the IOL in the posterior chamber, each end of the 10-0 prolene was suture fixated on the sclera (I, J). The corneal incision sites were closed by stromal hydration and conjunctival peritomy sites were tightly approximated with 8-0 vicryl suture (K). The suture knots of 10-0 prolene were securely placed underneath the conjunctiva and Tenon’s fascia (L).
The preoperative uncorrected distance visual acuity was 20/400 and this improved to 20/60 at 1 week after repositioning of the toric IOL. Preoperative corneal endothelial cell count was 3,020 cells/mm2 and it was 2,514 cells/mm2 at 1 week postoperatively. The IOL was well-centered and stable with its toric alignment within 5 degrees of the intended axis; 91 degrees (Fig. 4).
DISCUSSION
There are several reports of transscleral fixation using different types of toric IOLs in diverse situations [6-9]. They all suggested that good stabilization and visual rehabilitation can be achieved through transscleral fixation of the IOLs. Borkenstein et al [6] reported successful visual rehabilitation in an aphakic eye with high postkeratoplasty astigmatism using a Rayner 570T IOL. Emanuel et al [7] demonstrated scleral fixation of a single-piece AcrySof toric IOL without externalization of the haptics. McGrath and Lee [8] performed scleral fixation of a supplementary toric IOL (Sulcoflex toric 653T) by haptic externalization. In a situation of recurrent rotation of a toric IOL (Rayner 623T), Arjmand et al [9] fixated in-the-bag toric IOL sutured through the capsular bag to prevent IOL rotation.
In this case, the haptic was temporarily externalized through a small clear corneal incision. This is a closed-eye approach which minimizes intraocular manipulations to create a suture loop around the haptics and direct visualization of the haptics makes it easier to place the suture at the haptics [10]. This technique differs from the previous reports in the suture fixation point of the haptics. The knot was securely tied at the optic-haptic junction of the haptics just beside the toric markings, which enabled easier toric alignment at the desired axis. Also, the small notch at the optic-haptic junction prevented slippage of the knot along the haptic.
Single-piece acrylic IOLs have potentials for complications with sulcus placement; haptic-induced iris chafing can cause pigment dispersion, elevation of intraocular pressure, vitreous hemorrhage and cystoid macular edema [11-14]. In this case, the suture was placed more posteriorly (2-3 mm instead of 1 mm posterior from the limbus) to avoid these complications. No significant postoperative inflammation and no serious complications including choroidal hemorrhage, retinal detachment or endophthalmitis were observed in this case. Despite the floating suture due to the relatively long distance between the suture fixation point of the haptic and the sclera, the IOL was stable with good centration. Also, the 4-point fixation effect, since the haptic ends were placed at the ciliary sulcus, enhanced the stability of the IOL.
In summary, transscleral fixation can be considered in situations of late subluxation or dislocation of single-piece AcrySof toric IOLs. This technique is easy to learn, reduces surgical time with minimal manipulation and enables IOL stability with good postoperative toric axis alignment. However, further studies with larger series of cases and long-term follow-up is needed to fully evaluate the safety and effectiveness of this technique.
Notes
The author has no conflicts to disclose.
This study was supported by a Soonchunhyang University Research Fund.