Corneal Asphericity Variations in Korean Myopic Children
Article information
Abstract
Purpose
Corneal asphericity (Q-value) represents the difference in curvature from center to periphery of the cornea. This study evaluated horizontal and vertical asymmetry in corneal asphericity in myopic children and its relationship with various ocular parameters.
Methods
This retrospective study included 47 eyes in 24 myopic Korean children. Corneal parameters, such as corneal asphericity and thickness, apical radius of curvature, and high order aberrations including total root mean square (RMS), spherical aberration, coma, and trefoil were analyzed by Pentacam. Axial lengths (ALs) and anterior chamber depths (ACDs) were measured by IOL master. From these values, characteristics of corneal asphericity differences between nasal-temporal and superior-inferior quadrants in myopic children and their relationship with other ocular parameters were evaluated.
Results
The mean Q-value (8 mm) was -0.34 ± 0.10, representing a prolate corneal shape. The mean superior-inferior Q-value differences (8 mm) was 0.23 ± 0.17, which was greater than the mean nasal-temporal Q-value differences (8 mm) measured as 0.15 ± 0.13. The mean Q-value (8 mm) was not significantly related to AL or ACD, and Q-values in each quadrant (8 mm) also showed no significant relationship with corneal thickness in each corresponding quadrant. The nasal-temporal Q-value differences (8 mm) had a positive relationship with total RMS (p = 0.001) and a negative relationship with oblique trefoil (p = 0.045) and spherical aberration (p = 0.007). The superior-inferior Q-value differences (8 mm) showed a negative relationship with vertical trefoil (p = 0.003).
Conclusions
The results of the study showed a variation of nasal-temporal and superior-inferior Q-value differences, and the relationship between corneal shape and other ocular dimensions in myopic Korean children. Further study with large data set is merited to ascertain the epidemiologic data of Asian ethnicity.
INTRODUCTION
The anterior surface of the human cornea is a major refractive element, and it has been under numerous studies [1-3]. The corneal surface and shape are now described and investigated thoroughly as imaging techniques improved. A non-contact imaging technique such as corneal topography characterizes the shape of the cornea, especially the anterior surface of the cornea. The corneal topography developed from placido disk-based to scanning slit system and scheimpflug imaging [4]. This improvement in imaging techniques has led to greater accuracy and resolution in creating 3D map of cornea. As previous studies have discovered, the cornea is not a perfect sphere but its central part has a stronger curvature than its periphery [5]. The corneal shape can be described with corneal asphericity (Q-value), which represents the difference in curvature from center to periphery of the cornea [6,7]. Most of the human cornea shape flattens from corneal apex to periphery, showing a prolate ellipsoid shape [7-9]. The Q-value is used to specify the type of conicoid as described in Table 1 [10].
The corneal asphericity is associated with many clinical perspectives. Horner et al. [11] have shown that the peripheral cornea becomes more oblate (shift to a more positive Q-value) as myopia progressed. There is a study [12] indicating that in some patients, the corneal asphericity significantly changes as they age, and Davis et al. [10] also showed that the cornea becomes less prolate as children age. Xiong et al. [13] stated that the corneal asphericity shows a correlation with age, sex, and refractive power. Also, Namba et al. [14] suggested that astigmatism shifts toward against-the-rule as increase in age, and this change is associated with geometrical changes in cornea, especially the changes in the anterior surface of the cornea. In addition, the corneal asphericity is involved in treating patients. Previous studies [15,16] have shown that the corneal asphericity affects the refractive outcomes of intraocular lens (IOL) implantation. According to Li et al. [17], higher corneal asphericity differences between quadrants are related to contact lens decentration, which is the most common complication of treating myopic patients with orthokeratology lens.
Therefore, knowing the corneal asphericity and its relationship with other ocular parameters is crucial, but there are not many studies in this area with Korean ethnicity. The purpose of our study is to evaluate horizontal and vertical asymmetry in corneal asphericity in myopic Korean children and its relationship with various ocular parameters.
MATERIALS AND METHODS
This retrospective study included a total of 47 eyes in 24 Korean children with myopia who were candidate of orthokeratology lenses from May 2015 to September 2019 in Yeouido St. Mary’s Hospital. Subjects with a history of intraocular eyelid surgery, inflammatory diseases or ocular infection (viral, bacterial) were excluded. Patients with abnormal structural lesions were excluded via ophthalmic slit lamp microscopy and fundoscopy. The study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Catholic University of Korea Institutional Review Board (IRB) committee (SC19RISI0135). Informed consent from patients/legal guardians was waived because of the retrospective nature of the study.
Ocular parameters were collected from the patients before their orthokeratology treatment. Corneal parameters such as corneal asphericity (Q-value), corneal thickness, apical radius of curvature, and high order aberrations including total root mean square (RMS), spherical aberration, coma, trefoil were analyzed by OCULUS Pentacam® (Oculus, Wetzler, Germany). Axial lengths (ALs) and anterior chamber depths (ACDs) were measured by IOL master (Carl Zeiss Meditec AG, Jena, Germany).
From these values, a relationship between the corneal asphericity at 8 mm from the center in each quadrant and the corneal thickness in each corresponding quadrant was analyzed. The mean corneal asphericity and the corneal asphericity difference between nasal-temporal and superior-inferior quadrants at 8 mm from the center were calculated and their relationship with various other ocular parameters were evaluated.
Statistical analysis was performed using IBM SPSS Statistics for Windows (version 22.0; IBM Corp., Armonk, NY, USA). Data were expressed as mean ± standard deviation. Pearson correlation method was used to find the relation between the corneal asphericity difference measured by Q-value and other ocular parameters including total RMS (sum of RMS value of all higher order aberrations), spherical aberration, coma, and trefoil. In this study, correlation coefficient ‘r’ described the relationship between variables. A positive r value indicates a positive correlation and a negative r value a negative one. A r value also determines the strength of a correlation, which is r > 0.7 for a strong, r = 0.3-0.7 for a moderate, and r = 0.1-0.3 a weak correlation. A p-value < 0.05 was considered to be statistically significant.
RESULTS
The characteristics of the study subjects and ocular parameters are summarized in Table 2. The average age of the study subjects was 8.92 ± 1.32 years old. The average AL was 24.49 ± 0.69 mm, the average ACD was 3.68 ± 0.18 mm, and the average apical radius of curvature was 7.74 ± 0.25. The mean Q-value at 8 mm from the center was -0.34 ± 0.10, which showed a prolate ellipsoid shape of the cornea. The average Q-value difference between superior-inferior quadrants was 0.23 ± 0.17, which was greater than the average Q-value difference between nasal-temporal quadrants of 0.15 ± 0.13 (Table 3). The average high order aberrations were as follows: total RMS 1.46 ± 0.49, spherical aberration 0.19 ± 0.08, horizontal coma -0.04 ± 0.19, vertical coma -0.02 ± 0.15, vertical trefoil 0.00 ± 0.17, and oblique trefoil -0.03 ± 0.12 (Table 2).
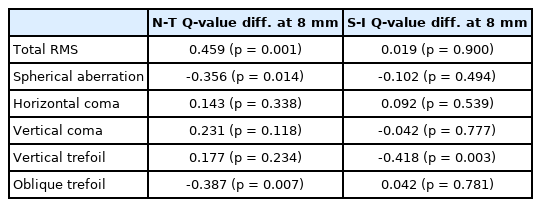
The mean Q-value at 8 mm showed no significant relationship with AL or ACD. The Q-value at 8 mm from the center in each quadrant and the corneal thickness in each corresponding quadrant were also not significantly related (Table 4). The relationship between the Q-value differences and the high order aberrations were analyzed in Table 5. The Q-value difference between nasal-temporal quadrants at 8 mm had a significant positive relationship with total RMS (r = +0.459; p = 0.001) and a significant negative relationship with spherical aberration (r = -0.356; p = 0.014) and oblique trefoil (r = -0.387; p = 0.007). The Q-value difference between superior-inferior quadrants at 8 mm showed a significant relationship with vertical trefoil (r = -0.418l p = 0.003) (Table 5).
DISCUSSION
In this study, the anterior cornea of myopic Korean children were analyzed by scheimpflug camera (OCULUS Pentacam®; Oculus). The analyzed mean corneal asphericity described a prolate ellipsoid shape of the cornea. The average Q-value difference between superior-inferior quadrants was greater than the average Q-value difference between nasal-temporal quadrants, which showed the horizontal and vertical asymmetry in corneal asphericity.
There have been quite a few studies on the relationship between the corneal asphericity and higher order aberrations. Our study stands out from other studies since it evaluated the relationship between the Q-value differences and higher order aberrations. González-Méijome et al. [18] suggested that the Q-values vary in different corneal regions. A single Q-value of anterior cornea could not precisely reflect the corneal structure and its asphericity, so we measured the Q-values at each quadrant and used these values to analyze the relationship with other ocular parameters.
In our study, the Q-value difference between nasal-temporal quadrant at 8 mm had a moderately negative correlation with spherical aberration (r = -0.356; p = 0.014) and with oblique trefoil (r = -0.387; p = 0.007). Total RMS and the Q-value difference between nasal-temporal quadrants at 8 mm showed a moderately positive correlation (r = +0.459; p = 0.001). Also, the Q-value difference between superior-inferior quadrants at 8 mm showed a moderately negative correlation with vertical trefoil (r = -0.418; p = 0.003).
Kasahara et al. [19] have shown that spherical aberration increases with high myopia, and Radhakrishnan and Aswathy [20] suggested that there is a strong negative correlation between spherical aberration and corneal asphericity, meaning the more prolate the cornea, the less the amount of spherical aberration. According to our study, the spherical aberration also had a negative correlation with the Q-value difference between nasal-temporal quadrant. This suggests that higher order aberrations, particularly the spherical aberration, can be influenced not only by the corneal shape whether they are prolate or oblate, but also by the asymmetricity of the anterior cornea.
Kiely et al. [21] indicated that the corneal asphericity and central corneal thickness had low correlation. Our study also showed that the corneal asphericity in each quadrant was not related to the corneal thickness in each corresponding quadrant. In addition, we found that there was no significant relationship between the corneal asphericity and AL or ACD. This result agrees with a previous study [10] that suggested there is no significant relationship between the contour of cornea and ACDs among myopes. However, our result is also contrary to what Wang and Bao [22] presented, that the eye with longer AL have a flatter cornea.
Additionally, our study data can be useful in prescribibng orthokeratology lenses. Orthokeratology uses rigid contact lenses to reduce the refractive error of myopia by flattening the cornea and reducing the corneal curvature during sleep [23,24]. Therefore, the shape of cornea which can be described as corneal asphericity is important for prescribing an orthokeratology lens successfully. Li et al. [17] suggested that higher corneal asphericity differences between quadrants are related to orthokeratology lens decentration. Our study showed that the Q-value difference between nasal-temporal quadrant at 8mm also had a correlation with higher order aberrations, especially with spherical aberration, total RMS and trefoil. Stillitano et al. [25] indicated that higher order aberrations are significantly affected during orthokeratology test. Based on these results, further studies on a correlation between lens decentration and higher order aberrations in orthokeratology are expected to be beneficial since lens decentration is the most common complication in orthokeratology.
Our study also some limitations. First, the study sample was not large enough to represent the general myopic Korean children and therefore to show more convincing conclusions. However, this was the first study to analyze the corneal shape with Q-values in myopic children of Korean ethnicity. Korea is a nation where prevalence of myopia and high myopia is high and increasing rapidly [26], so it would be beneficial to analyze the corneal shape of myopia children and how it changes as they age. The second limitation was that the study patients were not classified into degrees of myopia. Previous studies [19,20] have shown that there are differences in higher order aberrations according to degrees of myopia. So, our study could have had difficulties in accurately analyzing the relationship between Q-value differences and the higher order aberrations. Therefore, further study with more study subjects classified into degrees of myopia and follow up study as they age would be valuable to describe the characteristics of corneal shape more precisely.
In summary, the results of the study showed a variation of nasal-temporal and superior-inferior Q-value differences, and the relationship between corneal shape and other ocular dimensions in myopic Korean children. Considering these Q-value differences and their correlations with other ocular dimensions could help prescribing orthokeratology lens to children successfully. Further study with large data set is merited to ascertain the epidemiologic data of Asian ethnicity.
Notes
The authors have no conflicts to disclose.