Orbital Metastasis of Cervical Squamous Cell Cancer during Treatment with Pembrolizumab
Article information
Abstract
Purpose
This case report presents a rare occurrence of squamous cell carcinoma metastasizing to the orbit from the cervix.
Case summary
A 48-year-old female with cervical cancer and multiple bone metastases experienced binocular diplopia two days prior to admission to the Department of Gynecology for scheduled chemotherapy. She was undergoing treatment with pembrolizumab, a programmed cell death protein 1 (PD-1) inhibitor, for metastatic cervical cancer. The patient exhibited unilateral ptosis and restricted eyeball movement in the right eye. Brain MRI revealed a well-defined lobulated lesion attached to the superior rectus muscle in the right orbit and orbital apex. In suspicion of metastasis, radiation therapy with a dosage of 3,600 cGy was administered to the right orbital area, resulting in a reduction in size of the metastatic lesion. However, distant metastases subsequently developed in the bone and soft tissue, leading to the patient's demise one month later.
Conclusions
This report emphasizes the importance of considering orbital metastasis from cervical cancer in patients undergoing advanced stage chemotherapy. It highlights the rarity of such cases and underscores the need for heightened awareness of this malignancy in patients with underlying cancer.
INTRODUCTION
Cervical cancer ranks as the fourth most prevalent cancer among women. While cervical carcinoma commonly metastasizes to lymph nodes, bone, liver, and lungs, its occurrence in the orbit is rare. Orbital metastases typically originate from lung, breast, and prostate cancers [1]. In this context, we present a case of cervical squamous cell carcinoma metastasizing to the orbit, which is the first documented instance during treatment with a programmed cell death protein 1 (PD-1) inhibitor, pembrolizumab.
CASE
The study design followed the tenets of the Declaration of Helsinki for biomedical research and was approved by the Institutional Review Board of the National Cancer Center in Go-yang, Korea. Verbal informed consent was obtained from all authors to publish this information.
A 48-year-old female presented to the eye clinic with acute binocular diplopia that had manifested two days earlier. The patient had a prior diagnosis of cervical cancer, specifically International Federation of Gynecology and Obstetrics (FIGO) stage IIIC1, and had received concurrent chemoradiation therapy with cisplatin one year ago. However, despite concurrent chemoradiation therapy, the disease had progressed to involve multiple lymph node basins, including the retroperitoneal, axillary, and supraclavicular lymph nodes (Fig. 1). Consequently, the patient underwent six cycles of systemic chemotherapy comprising paclitaxel, cisplatin, and bevacizumab. The overall response to systemic chemotherapy was stable. However, two months later, disease progression occurred. Subsequently, the patient received combination therapy, including pembrolizumab. She reported experiencing blurred vision and diplopia that had commenced two days prior to presentation.

Axial fused FDG PET/CT showing multiple lymph node metastases in a 48-year-old woman with stage IIIC1 invasive cervical squamous cell carcinoma, non-keratinizing type. (A) Retroperitoneal area (arrow), (B) axillary area (arrow), (C) supraclavicular area (arrow).
Ophthalmic examination revealed binocular diplopia, limited eyeball movement, and ptosis in the right eye, with normal light response of the pupil. There was no evidence of eyelid swelling or pain. In suspicion of cranial nerve III and VI palsy, enhanced orbital magnetic resonance imaging (MRI) was conducted (Fig. 2). The brain MRI exhibited a well-defined lobulated lesion in the right orbit and orbital apex, displaying subtle enhancement and attachment to the superior rectus muscle of the right eye (Fig. 3). PET/CT and MRI confirmed the presence of orbital metastasis; however, the patient declined surgery for pathologic confirmation in the orbital area. Consequently, radiation therapy with a dosage of 3,600 cGy was administered to the right orbital area. The metastatic lesion in the right orbit decreased from 2.2 to 0.8 cm (Fig. 4). While the locally recurrent lesion in the cervix exhibited slight reduction with continued pembrolizumab treatment, distant metastases emerged in the bone and soft tissue, including the psoas and buttock. Palliative treatment was administered, but the patient expired one month after initiation of palliative care.
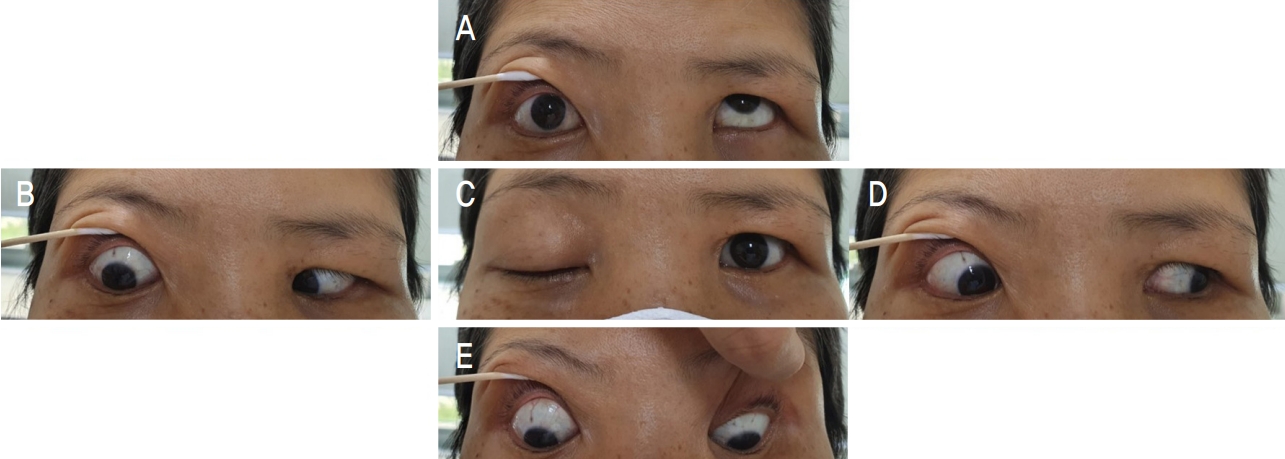
The photograph showing ptosis and extraocular muscle movement limitations of right eye at the initial examination. Complete ptosis of the right eye was observed at the first visit (C). Upward and sideward limitation of the eyeball was observed, although downward eyeball movement was preserved (A, B, D, E).
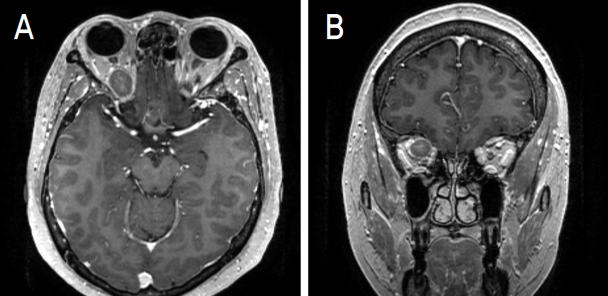
Initial brain MR image of the patient. (A) Axial MR T1 image of the orbit showing the well-defined lobulated lesion in the retrobulbar area up to the orbital apex of the right eye. (B) Coronal MR T1 image showing the possibility of attachment to the superior rectus of the right eye. MR, magnetic resonance.
DISCUSSION
Orbital metastasis from cervical cancer is an exceedingly rare occurrence, accounting for only 3-5% of all orbital tumors [1,2]. Hematogenous spread is considered the primary mechanism for orbital metastases, as the orbit lacks a lymphatic drainage system [3]. Additionally, blood flow in the ocular region comprises 2-5% of total circulation, exhibiting heightened activity within the intra-orbital space [4]. Consequently, tumor cells face difficulties surviving within this space, resulting in the rarity of orbital metastasis [5].
While cervical carcinoma predominantly metastasizes to lymph nodes, bone, liver, and lungs, only ten cases of orbital metastasis from cervical carcinoma have been reported to date [5-8]. Some previous studies have documented orbital metastasis concurrent with cervical cancer diagnosis [9]. The most common histopathologic type of orbital metastases from cervix is squamous cell carcinoma; most patients have stage 4 disease at the time of diagnosis [8]. The most common ophthalmic manifestation of cervical metastasis in the orbit is diplopia or proptosis, although eyelid swelling and visual loss have also been observed. Visual loss is generally caused by progressive orbital apex syndrome or choroidal involvement. Orbital metastasis should be considered if a patient with cervical cancer presents with extraocular muscle movement limitation [9].
This case stands out due to the detection of metastatic cervical squamous cell carcinoma during pembrolizumab treatment. Pembrolizumab, an immunotherapy agent targeting PD-1 on lymphocytes, is a humanized antibody commonly employed in the treatment of melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, and stomach cancer. The association between orbital metastasis and pembrolizumab remains unclear in this case. It is presumed that orbital metastasis was identified in a cervical cancer patient demonstrating disease progression despite pembrolizumab treatment.
A limitation of this study is that orbital metastasis was diagnosed based on radiological findings and ophthalmic manifestations, as pathologic confirmation was not feasible due to the patient's advanced stage cervical cancer and need for hospice care.
In conclusion, this case report presents a rare instance of orbital metastasis from cervical cancer. The report emphasizes the significance of considering this malignancy when encountering patients with orbital masses and underlying cancer.
Notes
The authors have no conflicts to disclose.
